In Vitro Fertilization (IVF/ET)
In Vitro Fertilization (IVF/ET) is an assisted reproductive treatment in which eggs and sperm are combined (fertilization) in a laboratory (“in vitro”) and then embryos are transferred to the uterus.
Before proceeding, we conduct in-depth studies on each member of the couple to recommend the appropriate treatment based on their specific situation.
Personalized evaluation.
We have a team of professionals ready to address all inquiries, and there is also the possibility to speak with our expert embryologist.
Our professionals.
Procedures
Depending on the quality of the semen sample, one of these two techniques will be recommended:
- Conventional IVF (In Vitro Fertilization): This is recommended for semen samples with mild abnormalities. A specific number of sperm is placed around each egg to allow one of them to penetrate and fertilize it.
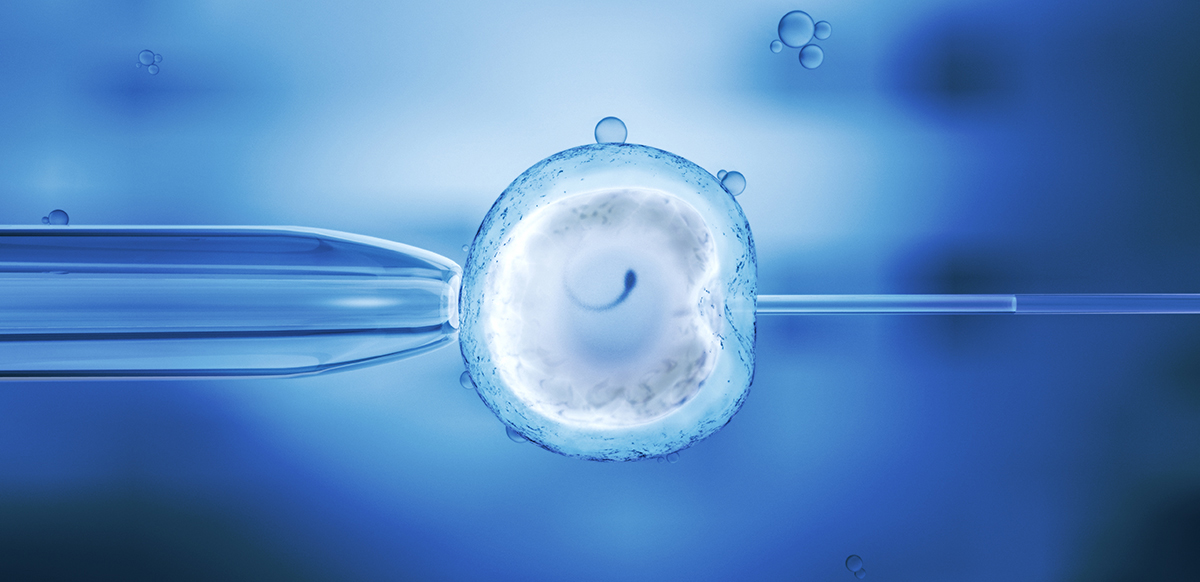
- ICSI (Intracytoplasmic Sperm Injection): In cases of a low quantity or quality of sperm, a single sperm is injected into the egg using a microscope with micromanipulation.
- Ovulation Stimulation
During a natural ovulatory cycle, typically, only one egg (oocyte) has the opportunity to be fertilized. Many of these eggs may have genetic abnormalities that prevent proper fertilization or development. The aim of ovulation stimulation is to recruit a greater number of eggs from both ovaries, increasing the chances of fertilization. Ovarian stimulation is achieved through hormonal medications (Gonadotropins) administered via subcutaneous injection. This process lasts about 10 to 12 days and may cause some discomfort, including a feeling of pelvic heaviness, mood changes, breast fullness, and, less commonly, nausea, dizziness, or headaches. The stimulation is completed with medications that prevent spontaneous ovulation (GnRH antagonists or progestins) since the extraction of eggs may be at risk if they are expelled from the body prematurely. During stimulation, between 3 to 6 transvaginal ultrasounds (ovulation monitoring) are performed to assess the growth and development of follicles, along with some blood tests to monitor hormone levels. When the majority of follicles reach an average size of more than 17-18 mm, human chorionic gonadotropin (hCG) or GnRH agonists are injected to complete egg maturation, and the follicular aspiration is scheduled 36 hours later. - Follicular Aspiration
This is the extraction of eggs from inside each follicle through ovarian puncture using a needle inserted vaginally and guided by ultrasound. The procedure is outpatient, with intravenous sedation, requiring at least an 8-hour fast from both solid and liquid food. The procedure usually lasts between 10 and 20 minutes. After the procedure, the patient rests in a recovery room for a short period and then continues resting at home for the remainder of the day. Starting on the night of the follicular aspiration or the following morning, as per the doctor’s guidance, the woman must begin daily hormonal progesterone supplementation. The most common route of administration is vaginal (in capsules or gel), and in exceptional cases, it can be given orally, subcutaneously, or intramuscularly. Hormonal supplementation continues daily until the pregnancy test (approximately 15 days), and if pregnancy occurs, progesterone supplementation is continued for another six weeks. - Semen Sample
The semen sample is obtained through masturbation. The semen is processed in the laboratory and placed in culture media to select the most suitable sperm for fertilization. In cases of azoospermia (absence of sperm in the semen), sperm may be obtained through testicular biopsy, a procedure called TESE (testicular sperm extraction), which requires a minor surgical intervention in the man. This can be done at the same time as the treatment or some time before, with the sperm obtained frozen. - Fertilization (IVF/ICSI)
Immediately after retrieval, the eggs are morphologically classified (based on their appearance) and by their degree of maturity. They are then fertilized through either IVF or ICSI and placed in an incubator. Fertilization is a process that begins with sperm penetrating the egg, continues with egg activation and the formation of pronuclei (two, one derived from the woman and one from the man), and ends with the dissolution of these pronuclei in a process called syngamy, leading to the division and multiplication of pre-embryonic cells. The evidence of successful fertilization is the microscopic visualization of pronuclei (male and female) 16 to 20 hours after co-incubation of both gametes (day 1). If the gametes are normal, the fertilization rate is approximately 70-80%. This rate varies depending on the morphological characteristics of the eggs and sperm, the woman’s age, and the cause of infertility. In cases where the quantity of eggs is very low or the quality of the gametes is very poor, there may be no fertilized eggs, and the procedure may need to be canceled. - Culturing and Development
After syngamy, the first two cells of the pre-embryo are formed (in high-quality embryos, this can be observed approximately 25 hours after the insemination of the eggs with sperm). Over the following days, the development of the embryos can be tracked to evaluate the number of cells and their characteristics. Typically, at 48 hours, you will see 4-5 cells, at 72 hours 7-8 cells, and by the 5th or 6th day, the blastocyst stage will be reached. According to the doctor’s judgment, the transfer can be performed at 72 hours (cleavage-stage embryo or day 3) or on the 5th day of development (blastocyst).

